: Admin : 2022-02-01
What is thyroidectomy?
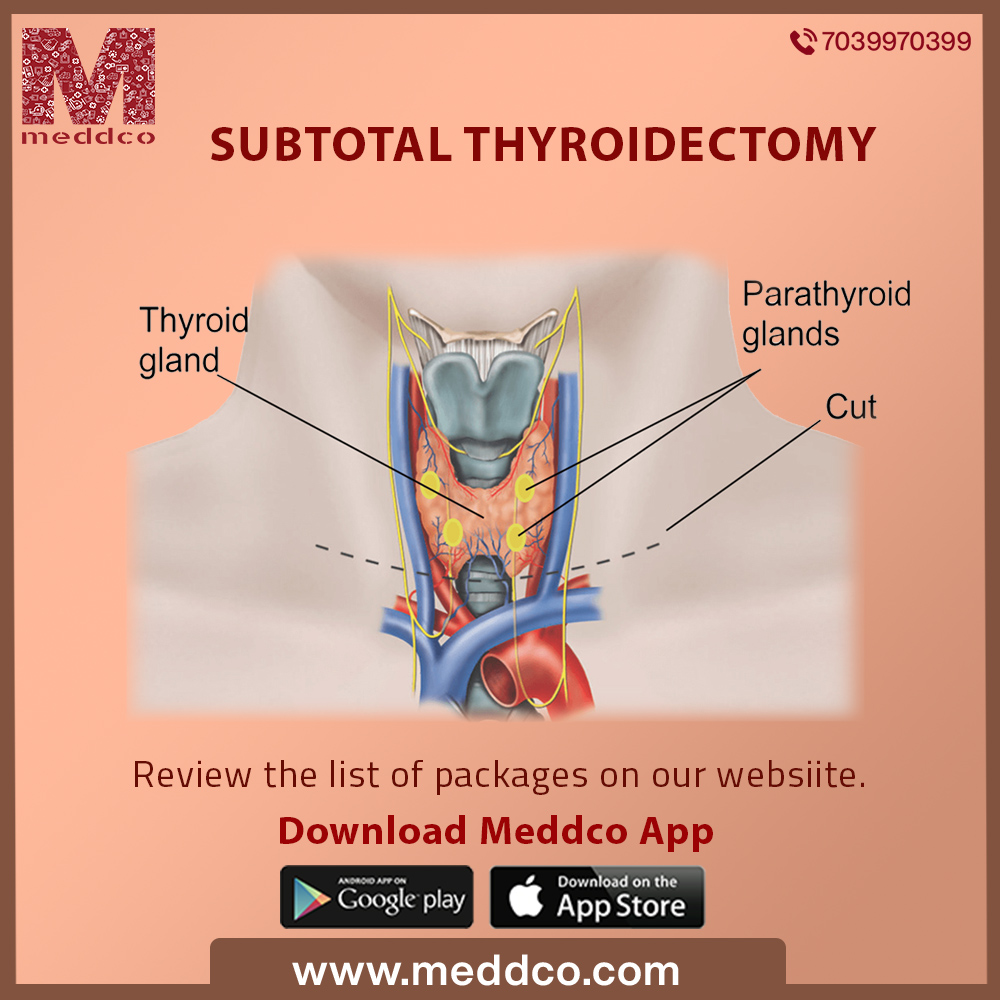
A thyroidectomy is an operation that involves the surgical removal of all or part of the thyroid gland.
The thyroid gland is a butterfly-shaped endocrine gland that is normally located in the lower front of the neck. The thyroid’s job is to make thyroid hormones, which are secreted into the blood and then carried to every tissue in the body. Thyroid hormones help the body use energy, stay warm and keep the brain, heart, muscles, and other organs working as they should.
Thyroidectomy can be classified into 5 distinct parts depending on the part of gland or whole of gland to be removed, the spread of the disease and type of disease. The different types of thyroidectomy are:-
Despite all the above classifications of the surgery, this article will mainly be focused to review, analyse and summarise Subtotal Thyroidectomy. However, the principles discussed may be applied to all Thyroidectomy procedures.
The thyroid gland releases thyroid hormone, which controls many critical functions of the body. Subtotal Thyroidectomy is usually performed to treat Grave’s disease, thyroid nodules, thyroid cancer, autoimmune (lymphocytic and hashimoto) thyroiditis, chronic lymphocytic thyroiditis etc. In simple words, this procedure is used to surgically cut out cancerous lumps and nodules on the thyroid gland. Other indications for surgery include cosmetic (highly enlarged thyroid), or symptomatic obstruction (causing difficulties in swallowing or breathing).
Subtotal thyroidectomy is also used to treat the thyroid gland when there is an excess secretion of thyroid hormone or hypothyroidism. Grave’s disease is one of the most common cause of this. Goiters which cannot be adequately managed with antithyroid medications (e.g., patients with toxic adenoma or toxic multinodular goiter) can also be removed with this procedure. Thyroidectomy can also be considered as primary therapy in refractory cases of amiodarone-induced hyperthyroidism.
There are few true contraindications to thyroidectomy. Given that thyroid cancer is generally a slowly progressive disease, the risk/benefit profile changes with age and this should be discussed with patients who are considering undergoing thyroidectomy.
Anaplastic carcinoma represents a treatment dilemma due to its poor outcomes and propensity for rapid progression. Surgical resection may be offered if gross total resection can be achieved with minimal morbidity and there is no evidence of metastases. Surgical intervention may otherwise be contraindicated.
Surgical factors considered relative contraindications to outpatient surgical management include massive goiter, extensive substernal goiter, locally advanced carcinoma, challenging hemostasis, and a difficult thyroidectomy in the setting of Hashimoto's or Graves' disease.
Once it is determined that you need surgery, the doctor do a physical neck and head check and run tests on you like a CT scan and PET scan and blood tests. He will make sure to check your vocal cords by indirect laryngoscopy to rule out any unsuspected pre-existing unilateral nerve palsy, this is particularly important if the patient has undergone any previous thyroid surgery. These tests will confirm the location and type of cancer. They will also indicate if the patient is healthy enough to pull through with the surgery. Patients should be rendered euthyroid with antithyroid drugs before surgery.
If you have hyperthyroidism, your doctor may prescribe medication — such as an iodine and potassium solution — to control your thyroid function and lower the bleeding risk after surgery.
Generally, patients should not eat or drink anything except essential medications after midnight before the surgery. This is because when the anaesthetic is used, your body's reflexes are temporarily stopped. If your stomach has food and drink in it, there's a risk of vomiting or bringing up food into your throat which can cause complications during the surgery. Patients should inform their doctors in case they feel sick, nauseous or uncomfortable.
Essential personnel for this procedure include the primary surgeon, 1 or 2 surgical assistants, a circulating/operating room nurse, a surgical technologist, and an anesthesiologist and most importantly, the patient. Airway management should be discussed with the anesthesiologist prior to starting the procedure. The personnel can also depend on kind of procedure, availability etc.
An uncomplicated subtotal thyroidectomy should take less than 2 hours to perform. If you are having a less extensive operation, it will be quicker. During the surgery, your surgeon may use the NIM® Nerve Integrity Monitoring System from Medtronic to help reduce the risk of nerve injury to the nerves controlling your voice. The NIM allows the surgeon to locate the nerves that run close to your thyroid and also to test their functioning during surgery, thereby reducing the risk of damage.
In a subtotal thyroidectomy, the surgeon will make an incision
Thyroidectomy is a common surgical procedure that has several potential complications or sequelae including: temporary or permanent change in voice, temporary or permanently low calcium, need for lifelong thyroid hormone replacement, bleeding, infection, and the remote possibility of airway obstruction due to bilateral vocal cord paralysis. Complications are uncommon when the procedure is performed by an experienced surgeon. But, like every surgery, subtotal thyroidectomy can have several complications. The most important complications of thyroidectomy are listed as follows:
The recovery time for a subtotal thyroidectomy is anywhere from 2-3 days, more in case of additional surgeries due to complications. The patient is usually fed via a tube in the recovery period. Ample of rest is advised as long as it is not painful. There may be a change in diet and your care team will give you thorough instructions on how to care for your incision sites and what to do in case of emergencies.
Patients are asked to take 1000 mg of calcium 4 times a day for the first week after surgery and then 500 mg of calcium twice a day for the next 2 weeks until their post-operative visit to help avoid the symptoms of low calcium levels. After the removal of a thyroid, patients usually take a prescribed oral synthetic thyroid hormone, levothyroxine (Synthroid) to prevent hypothyroidism. Patients may have a gauze pressure dressing around your neck. The doctor will give instructions on when to remove it. The stitches in the incision will need to be removed in 5-7 days, or patients may have dissolvable stitches that do not require removal. If the incision has been closed with dissolvable stitches, the patient will likely have either skin glue or paper tapes (Steri-Strips) covering the incision. Some people may need to have a drain placed under the incision in the neck. This drain is usually removed the morning after surgery. After thyroidectomy, a few people may experience neck pain and a hoarse or weak voice. This doesn't necessarily mean there's permanent damage to the nerve that controls the vocal cords. These symptoms are often short-term and may be due to irritation from the breathing tube that's inserted into the windpipe during surgery, or be a result of nerve irritation caused by the surgery.
You'll be able to eat and drink as usual after surgery. Depending on the type of surgery you had, you may be able to go home the day of your procedure or your doctor may recommend that you stay overnight in the hospital. When you go home, you can usually return to your regular activities. Wait at least 10 days to two weeks before doing anything vigorous, such as heavy lifting or strenuous sports. It takes up to a year for the scar from surgery to fade. Your doctor may recommend using sunscreen to help minimize the scar from being noticeable.
Thyroidectomy is an important surgical procedure with high-quality evidence for the management of benign and malignant thyroid disease. Due to the close proximity of several critical anatomic structures, safe thyroidectomy requires detailed anatomic knowledge and careful patient selection is paramount.
subtotal thyroidectomy treatment surgery
No Comments