: Admin : 2022-01-31
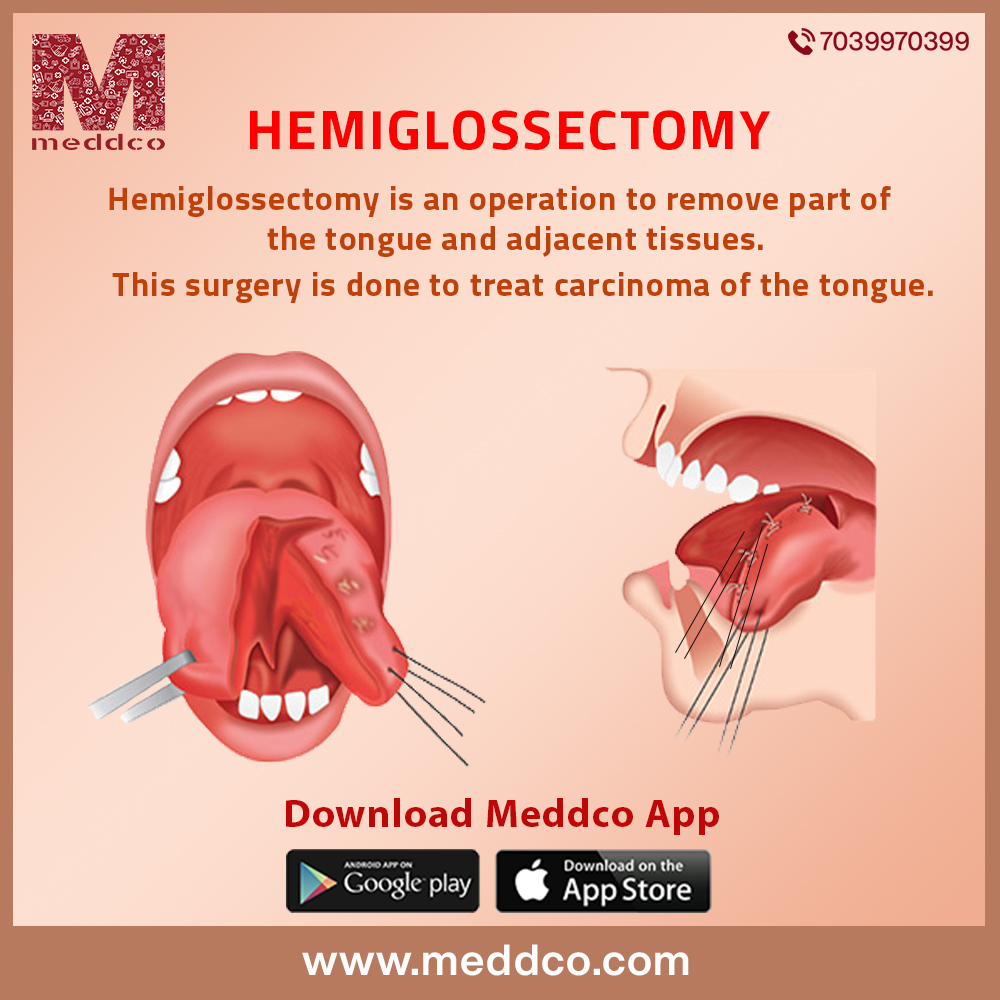
What is hemiglossectomy?
A hemiglossectomy is the surgical removal of all or part of the tongue. If the tumour is in the tongue, resection of the tongue may be necessary. Depending on the size of the tumour, partial resection or hemisphere resection is performed. This means that part or half of the tongue has been resected. Surgery to remove part of the tongue and surrounding tissues. A hemiglossectomy may be done to facilitate breathing after surgery, and skin grafts may be needed to replace the removed tissue. It is performed under general anaesthesia and the procedure can take several hours. It usually requires a long hospital stay. In some cases, The entire tongue is removed. This prevents food/liquid from entering the lungs and making it impossible to swallow (called aspiration). For this reason, a laryngectomy may be performed. A laryngectomy (removal of the larynx or larynx) helps prevent aspiration but also results in loss of voice. This type of hemiglossectomy also requires reconstructive surgery. Depending on the surgery, temporary or permanent tracheostomy may be required. Your care team can talk to you about whether and how long you need it. Your doctor will tell you about the features of the surgery.
Risks and Benefits
Before your surgery, your care team will discuss your health and other risks associated with the specific surgery you will have.
Why is it going on?
If a malignant tumour is found in the tongue, a hemiglossectomy may be performed. Diagnosis depends on microscopic examination of cells obtained by biopsy (collection of tissue). Critical treatment decisions are based on the process of determining the stage, the degree of primary growth of the tongue, and the presence of metastases (metastasis) to other parts of the body. An evaluation may include x-rays, computed tomography of the neck and liver, and biochemical studies. You may need a graft to replace the tissue removed during surgery. If only skin covering is required, a thin layer of skin (a split skin graft) may be taken from the thigh and applied to the wound. If tissue loss is greater, full-thickness grafts of skin, underlying muscles, and blood vessels from the chest, back, or forehead may be taken and used to reconstruct the tongue and mouth.
Procedure
Preparation for Surgery
You may be admitted to the hospital several days before your surgery. You will undergo a thorough physical examination and blood and urine samples will be taken for analysis. Your dentist will carefully examine your mouth. Bad teeth are removed before surgery to eliminate potential sources of infection. During surgery, it may be necessary to remove a healthy incisor or canine on the affected side to improve access to the mouth. If transfusion is required, cross-compatibility is performed. If you are anaemic or have lost a lot of weight, you may be hospitalized to improve your pre-operative condition. This may include blood transfusions and intravenous nutrition. A physical therapist may visit you and show you some breathing exercises that will continue after surgery to reduce your risk of post-operative complications. Medical and nursing staff will discuss your post-operative care with you. The night before surgery, you should shower or bathe and wash your hair. A tongue resection is a surgery to remove part or all of the tongue. It may be used to treat cancer of the tongue, certain types of cancer of the mouth (in the mouth), and throat. The action of the tongue includes tasting, swallowing, breathing, licking, and speaking.
On the day of surgery,
there was nothing to eat or drink since midnight. A second shower or bath may be requested. All makeup, jewellery, and dentures must be removed before going to the operating room for a hemiglossectomy. You will receive a pre-injection to help you relax an hour before surgery. The superficial topography of the tongue includes the tip of the tongue, the lateral, ventral tongue, the dorsal tongue, and the base of the tongue. The tip of the tongue represents the very front of the tongue. The lateral edge of the tongue separates the dorsal and ventral surfaces of the tongue. The ventral tongue is the lower surface of the tongue and the dorsal tongue is the upper surface. The base of the tongue is the posterior third of the tongue. It contains the tongue tissue behind the trough papilla that extends into the vallecula (the latter is the area between the base of the tongue and the epiglottis). Language can also be described in thirds. The tip of the tongue is the anterior third of the tongue. The middle third is between the tip and base of the tongue. The anterior two-thirds of the tongue is considered part of the oral cavity and the base of the tongue on the posterior third is considered part of the oropharynx.
The tongue has eight pairs of muscles. The muscles of the tongue are divided into internal and external. Their muscles have no attachment or origin outside the tongue. They are limited to the body of the language. Their actions shape language, but do not change the position of language. They are named after the direction they run: the upper and lower longitudinal muscles, the transverse muscles, and the longitudinal muscles. Four external muscles attach to the body, starting on the outside of the tongue. These muscles change the position of the tongue and include the gluteus maximus, palatal, and palatine muscles.
In the operating room
The surgeon works in a supine position under anaesthesia with the neck extended. A hemiglossectomy may be performed prior to the procedure. In hemiglossectomy, an incision is made under the mandible on the side of the lesion. Sometimes the incision must extend to the chin and lower lip. The lower jaw is cut to provide good access to the bottom of the mouth. The surrounding edges of the tumor and healthy tissue are removed. When this is done, the surgeon secures the mandible with an internal wire. If a graft is needed, it is taken from the donor site and sutured in place. A full-thickness graft is first left attached to the donor site to maintain a good blood supply while the graft is healing. The donor site of the free graft is covered with a sterile dressing. The incision is closed and drainage is inserted into the wound to prevent fluid build-up and improve healing. After you are released from anaesthesia, you will be briefly moved to the recovery room for observation. A hemiglossectomy is performed to provide oxygen and fluids by vein. A nasogastric tube may be inserted. You may be transported to the intensive care unit to observe and continuously monitor vital signs (pulse, body temperature, blood pressure, respiration) for several hours. You may feel drowsy, sore, and nauseous. Analgesic injections and injections for nausea are given as needed. You cannot speak while the hemiglossectomy tube is in your neck. You can communicate by providing a Magic Slate or pencil and paper.
Back in your room
Elevates the head and shoulders to reduce swelling and make swallowing easier. The frequent aspiration and repositioning of hemiglossectomy prevent the accumulation of secretions in the airways. Saliva may be sucked out of your mouth. You will be asked to get out of bed as soon as possible. Your physical therapist can continue the exercise. Health care providers keep your mouth clean to promote healing and make you more comfortable. Nasogastric feeding continues until you can eat normally. When the swelling in your mouth subsides, a speech therapist can help you restore normal speech. A few weeks after surgery, the full-thickness graft can be separated from what is attached to the donor site. Additional skin grafts may be required to close the donor site. Once the transplant has healed, you can go home.
Travelling home
When you are discharged, you will make an appointment with your surgeon for a post-operative check-up. Light exercise, but with adequate rest and balance. It is recommended to avoid unnecessary bending and lifting weights. Regular and thorough oral care is essential, and we will tell you how. It is recommended to eat light meals for several months to prevent damage to the graft and allow the jaw to fully heal. There are times when dentures cannot be worn. Speech therapy is continued for as long as necessary. It takes time to accept surgery that affects your appearance. A consultant or member of a patient support organization may visit you.
Possible Complications
If the tongue begins to bleed after surgery, emergency surgery may be required. Bad teeth can prevent or delay the healing of the mandible. In this case, antibiotics are prescribed and the tooth is removed. In rare cases, it may be necessary to re-immobilize the chin. Graft failure can be caused by an infection and is treated with antibiotics. A second transplant may be necessary if the graft's blood supply is insufficient.
Types of hemiglossectomy:
Reason for surgery:
This surgery is used to treat tongue cancer when other treatments have failed. Tongue removal is indicated if the patient has cancer that does not respond to other treatments. However, in most cases, only part of the tongue is removed (partial glossectomy). Tongue cancer is considered very dangerous because it can easily spread to surrounding lymph nodes. Most oncologists recommend surgical removal of the cancerous tissue.
What is recovery?
Recovery after a tongue resection depends on the type of surgery you have. A hospital stay of 7-10 days is often required. Temporary or permanent feeding tubes may be required to feed during and after the healing process.
Before leaving the hospital, you will learn how to care for the incision and other instructions. Your doctor will talk to you about whether you need diet changes, feeding tube and/or tracheostomy management, rehabilitation, and/or speech therapy. Your care team will talk to you about any medications you will be taking (eg pain, blood clots, infections, constipation prevention, and/or other conditions). Your doctor will tell you about any changes in your activity level that depend on your surgery.
What do you need at home?
Thermometer to check the temperature that may be a sign of infection.
Wound care supplies, feeding tubes, and tracheostomy orifices as needed.
When should I call a doctor?
Your doctor will give you details on when to call the office. It is advisable to contact your doctor if:
Be sure to take prescribed medications to prevent pain, infection, and/or constipation. Call the team if you have new or worsening symptoms. There are ways to deal with constipation after surgery. Talk to your doctor before taking any medications for constipation. Deep breathing and rest can help manage pain, keep the lungs healthy after anaesthesia, and facilitate lymphatic drainage. For the first week, try deep breathing and relaxation exercise a few times a day or when you're too nervous. Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow, deep breaths. Relax your muscles. Slowly turn your head and shoulders.
Diseases are never meant to get ignored. So contact us just now and get your treatments done with us. We give you a beautiful environment and a good treatment to help to get a healthy life and tips for quick recovery.
hemiglossectomy surgery tumour
No Comments