: Admin : 2022-09-23
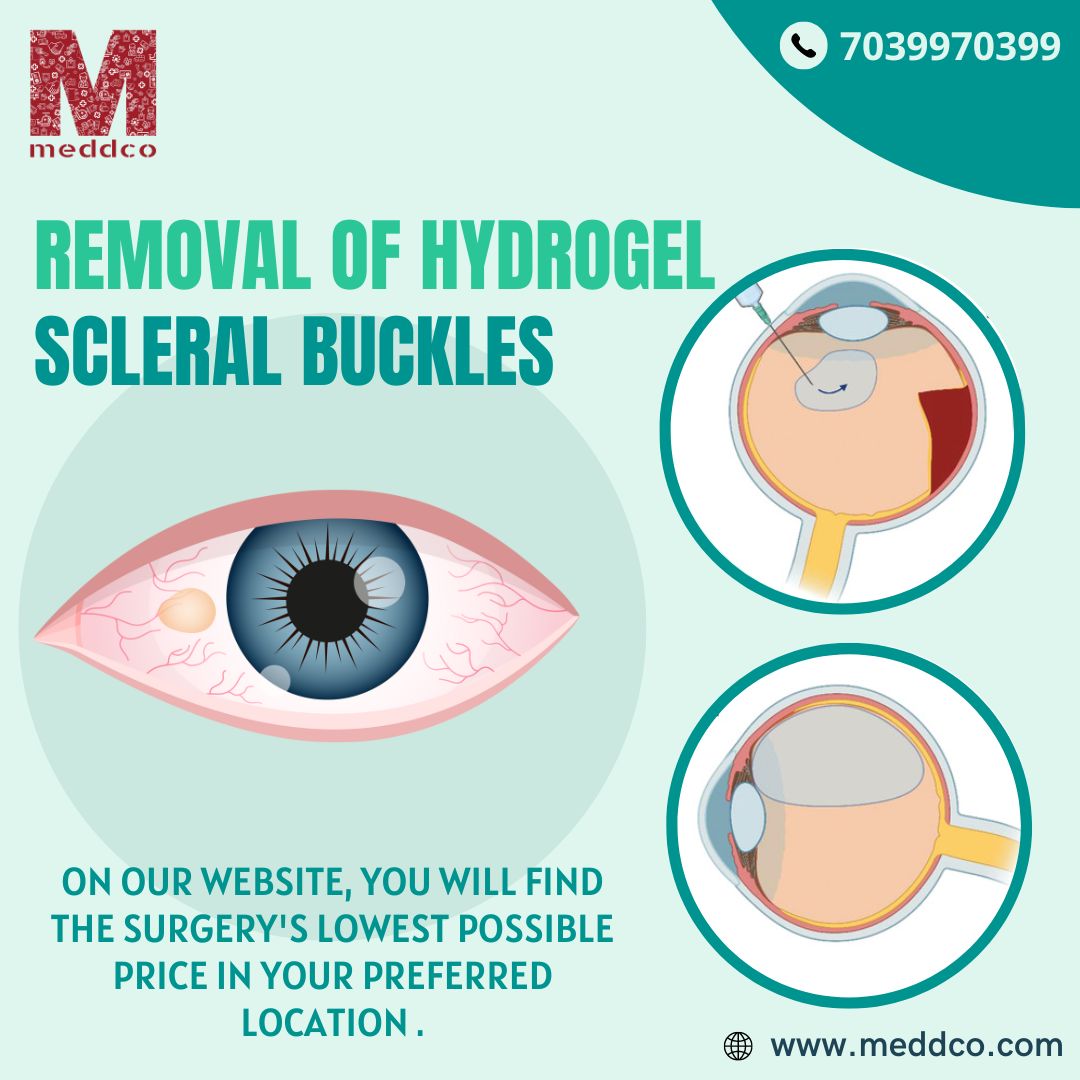
Today, ophthalmologists in general, and retina surgeons in particular, continue to see patients who present with symptoms related to hydrogel buckle swelling. When swelling becomes symptomatic, surgical removal is usually the only option for symptom relief. Unfortunately, removal is not without risks. Surgeons must recognise the presenting symptoms and be aware of the friable characteristics of this material as well as the risks associated with removing these hydrogel buckles when planning surgical removal.
SYMPTOMS
SURGERY TECHNIQUE
SURGICAL REMOVAL RISKS
eye eye surgery treatment hydrogel buckle
No Comments