: Admin : 2022-01-27
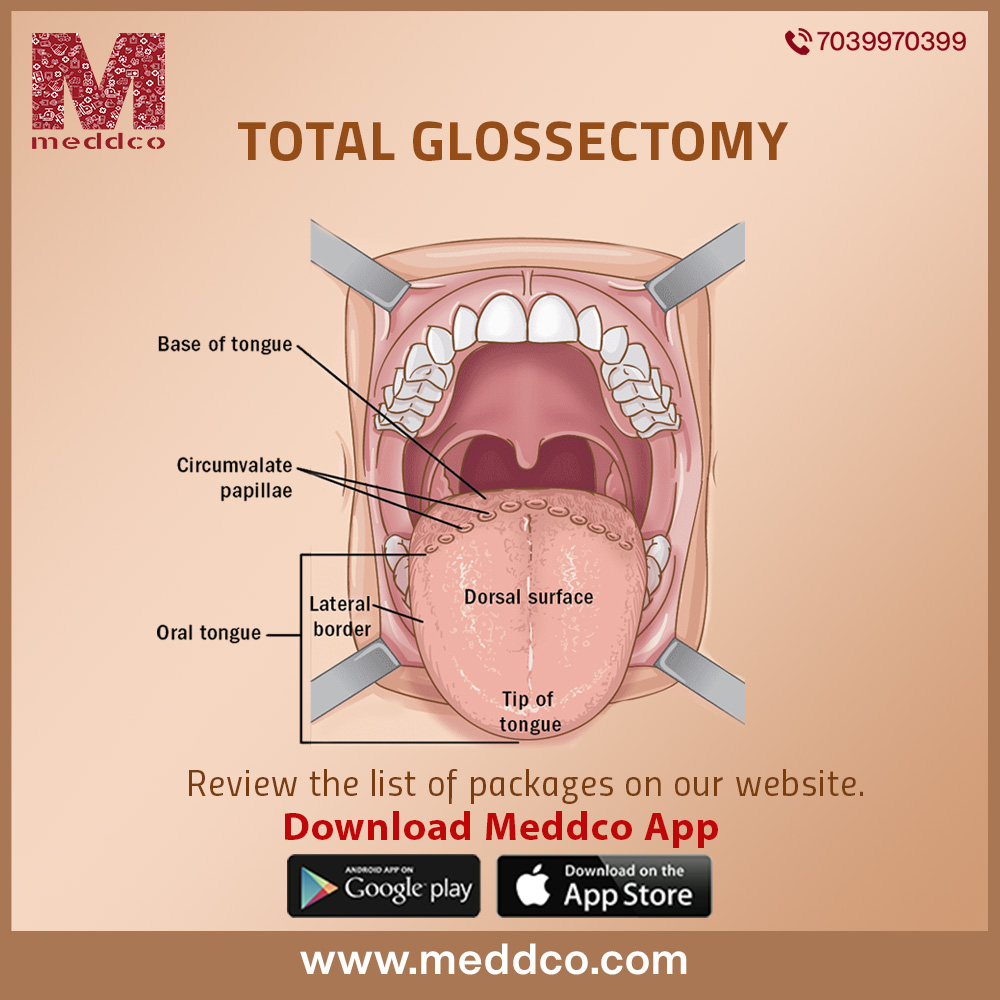
Total Glossectomy
Glossectomy is a surgical procedure that involves the removal of part or all of the tongue.
Glossectomy can be classified into different parts depending on the type and spread of cancer and the portion of removal of cancer from a tongue or oral cavity. The different types are:- The different types are:-
In partial glossectomy, only less than one half of the tongue is surgically removed. It is usually a small portion like a corner or the tip.
Hemiglossectomy is the surgical removal of half of the tongue. This surgery is performed for larger tumours.
Subtotal glossectomy is the surgical removal of more than half but less than total glossectomy i.e complete removal of the tongue.
Total glossectomy is the surgical removal of the entire tongue, including the base of the tongue. A total glossectomy may be performed along with a total laryngectomy (removal of voice box and pharynx) in order to prevent aspiration (breathing food or drink into lungs) and pneumonia. A total glossectomy will require major reconstructive surgery.
Despite all the above classifications of the surgery, this article will mainly be focused to review, analyse and summarising Total Glossectomy. However, the principles discussed may be applied to all glossectomy procedures.
This procedure is most commonly used to treat malignant or pre-malignant tongue lesions, or in simple words, cancer on the tongue and in and around the oral cavity. Malignant lesions have the ability to spread via the bloodstream or lymphatic system and thus it is preferred to nip them in the bud. It is the most common sleep-related breathing disorder.
It can also be performed for macroglossia, benign neoplasms of the tongue and obstructive sleep apnea. Obstructive sleep apnea (OSA) is a disorder caused by the repetitive collapse of the upper airway during sleep. It is the most common sleep-related breathing disorder. OSA occurs when the muscles supporting the soft tissues in your throat, such as your tongue and soft palate, relax.
First and foremost, your doctor will do a physical examination of your head and neck and then run several tests like a PET scan, MRI and a CT scan on you to confirm that you are ready for surgery and will pull through. After that usually, your doctor or care team will give you specific instructions on what to do and how to prepare for your surgery. The different types are:-
Generally, patients should not eat or drink anything except essential medications after midnight before the surgery. This is because when the anaesthetic is used, your body's reflexes are temporarily stopped. If your stomach has food and drink in it, there's a risk of vomiting or bringing up food into your throat which can cause a problem during surgery. Patients should inform their doctors in case they feel sick, nauseous or uncomfortable.
Patients should also be physically and mentally prepared for changes in the way they talk, eat and swallow after surgery. The extent of change will depend on the type and spread of cancer or malignant lesions, the approach used during surgery, complications of the surgery, and the reconstruction performed to replace the tongue. The different types are:-
Essential personnel for this procedure include the primary surgeon, 1 or 2 surgical assistants, a circulating/operating room nurse, a surgical technologist, and an anesthesiologist. Airway management should be discussed with the anesthesiologist prior to starting the procedure. The different types are:-
A total glossectomy can be done with a few different approaches depending on which part of the tongue the surgeon will operate on, how much is to be removed and what are the other associated procedures. The different approaches used are listed below:- The different types are:-
This approach is used for the small malignant lesions of the mouth. Here, the entire surgery can be done through the mouth.
This approach is usually used for tumours at the base of the tongue. Here, a robotic-assisted surgical removal takes place through the mouth.
A laryngoscope is placed through the mouth to expose various parts of the base of the tongue. A laser then cuts around the tumour and removes it. The different types are:-
This method is used specifically for tumours in the back part of the tongue or its base. Here, the surgeons make a cut in the middle of the jaw bone and move it to the side, effectively exposing the back of the tongue and the floor of the mouth. Later, the jaw is put back into place and aligned with plates and screws.
This approach also helps to expose the base of the tongue. An incision is made in the pharyngeal wall, providing access to the pharynx via an anterior pharyngotomy. The surgeon can now access the base of the tongue and the oropharynx. This procedure has become seemingly popular over the years as it gives excellent exposure to lesions and the surgeon does not need to cut the jaw in half like in a mandibulotomy.
Just like any surgery, glossectomy has many potential risks. Since it is a surgical head and neck procedure, some of the complications are listed below:-
Just like surgery, general anaesthesia also has complications, though remote, the patient should be aware of. They are cardiopulmonary events, strokes or even death. The different types are:-
As with any procedure, there are risks in undergoing a glossectomy that patients need to be aware of. The smaller the region of the removed tongue, the lesser the chance of many of these complications are, especially difficulty with speaking and swallowing. The following are the risks:-
Aspiration is a condition in which food, liquids, saliva or vomit is breathed into the airways. Risk factors include surgery, being less alert due to medication or illness and drinking large amounts of alcohol. Pulmonary aspiration may lead to pneumonia or death by suffocation.
Symptoms include coughing, difficulty breathing and in some cases choking. The different types are:-
Treatments include making sure the airway is open, close observation and, in case of infection, antibiotics. The different types are:-
The recovery time for a total glossectomy is anywhere from 7-10 days, more in case of additional surgeries due to complications. The patient is usually fed via a tube in the recovery period. There may be a change in diet and your care team will give you thorough instructions on how to care for your incision sites and what to do in case of emergencies. You will also be advised speech therapy and rehabilitation to help talk, eat and function of speech. Medications vary for different patients and will depend on your pain levels, allergies etc. Medications will also be given by doctors for different scenarios like blood clots, infections, constipation etc.
Speech Therapy Depending on the extent of your glossectomy and the sensation and movement of your residual tongue, you will likely work with a speech therapist to resume speaking and swallowing after your surgery. They will work with you to improve tongue function and the understandability of your speech. A key point in rehabilitation is postoperative speech and swallow therapy to improve the functional outcome following total glossectomy with laryngeal preservation. A study by Dziegielewski et al. reported superior speech and functional outcomes in patients who attended more than 80% of swallowing and speech rehabilitation sessions.
glossectomy total glossectomy
No Comments